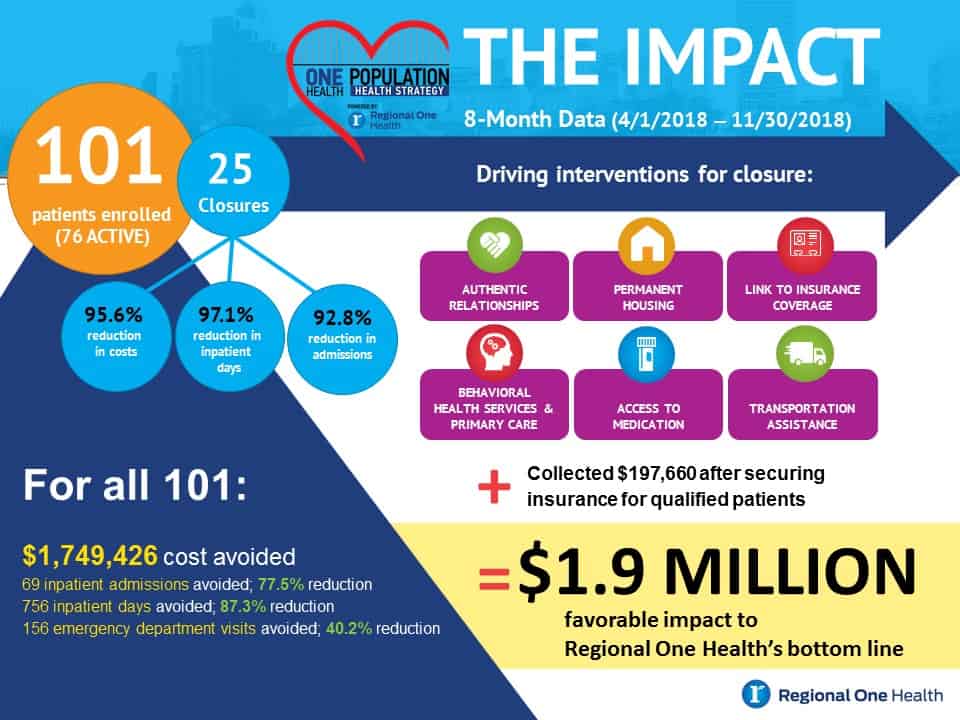
 ONE Health, led by Regional One Health Senior Vice President and Chief Integration Officer Susan Cooper and Project Manager Megan Williams, has served 101 people since April 1 of this year. Seventy-six remain active and 25 people have graduated from the program.
ONE Health, led by Regional One Health Senior Vice President and Chief Integration Officer Susan Cooper and Project Manager Megan Williams, has served 101 people since April 1 of this year. Seventy-six remain active and 25 people have graduated from the program.
For the 25 graduates, ONE Health has realized a decrease of 95.6 percent in costs, 97.1 percent decrease in inpatient days, and a 92.8 percent decrease in admissions.
For all 101 patients, ONE Health has resulted in avoiding $1.75 million in costs, along with 69 fewer inpatient admissions, 756 fewer inpatient days and 156 fewer emergency department visits. Combined with collecting $197,000 after securing insurance for qualified patients, the total benefit to Regional One Health’s bottom line was $1.95 million.
Those numbers are putting Regional One Health on the forefront of the complex care field, and in 2019 the hospital will cohost the National Center for Complex Health and Social Needs “Putting Care at the Center” conference Nov. 13-15.

“Most importantly, we’ve been able to really make a difference in people’s lives, and take people from being hopeless to having hope.” – Susan Cooper
“Regional One Health is payer and provider for uninsured patients, so any way you can increase their health and connect them to services bends the cost curve and improves both health and finances,” Cooper said, adding there are also societal benefits, like reducing homelessness and freeing up hospital resources. “Most importantly, we’ve been able to really make a difference in people’s lives, and take people from being hopeless to having hope.”
Regional One Health President and CEO Reginald Coopwood, MD said it’s the human impact that is truly inspiring. “The economic impact is valuable, but the stories have much more value to me,” he said. “They’re doing things to help people live healthier and more productive lives.”
Take an exhausted man Williams approached in Regional One Health’s emergency department.
When she offered to help, he followed her not because he believed she could improve his reality of living in abandoned buildings and enduring the pain of untreated cancer, but because he couldn’t summon the will to resist. Today, he is undergoing cancer treatment, lives in safe senior housing, and has disability benefits and income from early retirement and Social Security.
Williams had changed – and probably saved – his life. “When I met him, he was exhausted, and I promised to help,” she said. “Recently he told me, ‘I didn’t believe you, but I was tired and I didn’t have anything left in me but to follow you.’ Today, he’s doing amazing.”
For the ONE Health team, the man’s story is the sort that plays out daily. “No one wakes up and says, ‘I want to be sick, homeless and poor,’ but society places labels and blame,” Cooper said. “However, if you ask people their story and listen with an open ear, you can understand what they need and how to help. It’s about honoring their lived experience.”
ONE Health uses Regional One Health’s resources and commitment to compassionate care to keep those individuals healthier and address how a small fraction of users account for an outsize percentage of costs – an issue that has gone unaddressed for too long: “Every day, someone says to us: ‘No one has ever taken the time to listen to me and genuinely care for me,’” Williams said.
The ONE Health team listens, they care, and they take action. “You have to treat the person first before you can treat the healthcare needs,” Cooper said, because no two patients are the same. “When someone has a condition like diabetes, there is a recognized standard of care. For people who are complex, there is no single standard of care.”
She cited a quote from Coopwood that started trending on Twitter after he spoke at this year’s Putting Care at the Center conference: “There is no app you can build to manage people with very complex needs.”
Patients become super-utilizers due to fragmented care, chronic disease, mental health issues, poverty, etc., and to qualify for ONE Health, they must be uninsured and have had four or more hospital stays or 10 or more emergency department visits in two years.

Project Manager Megan Williams speaking about her passion in helping those who have become superusers of the healthcare system, “You have to dig through the layers and they have to hear your heart,” she said. “When they do, they trust you.”
Some patients are referred by internal medicine or emergency staff, but often Williams seeks them out – checking admission lists and intervening where needed. When she connects with a patient, she reviews their 10-year chart and does a root cause analysis of why they are a super-utilizer: “You’re looking for not only patterns of use, but patterns for reasons for use.”
Then, ONE Health works by connecting them with not only healthcare but resources in the community that provide or assist with housing, transportation, food, etc. Moving forward, the ONE Health team, with support from the Regional One Health Foundation and generous donors including The Assisi Foundation, will look to expand their reach by adding staff to serve even more patients while adding to their network of community resources and partners.
Williams said the latter means outreach to other local organizations that can help meet a variety of patient needs: “We need to find more partners in the community,” she said.
And, of course, they also need to continue to do what Williams did when she encountered an exhausted man in the ER: Offer to help, follow through, and erase doubt and mistrust. “You have to dig through the layers and they have to hear your heart,” she said. “When they do, they trust you.”
To read part two of our One Health Update, please click here.